In a landmark study that could reshape our understanding of autism treatment, researchers have demonstrated significant improvements in social behaviors in mouse models through targeted gene therapy. The findings, published this week in Nature Neuroscience, represent one of the most promising therapeutic approaches to address core symptoms of autism spectrum disorder (ASD) at the biological level.
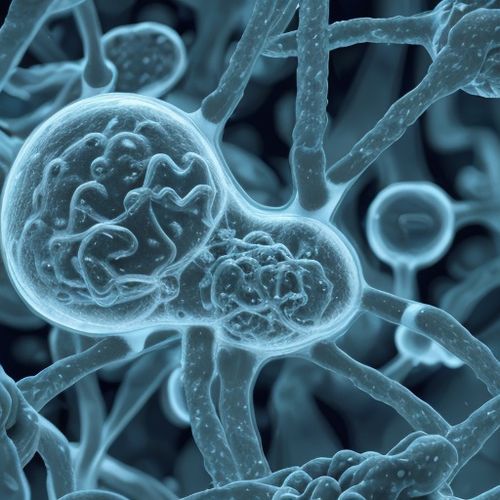
The international research team focused on correcting mutations in the SHANK3 gene, one of the highest-confidence autism risk genes that plays a crucial role in synaptic function. Approximately 1% of people with autism carry mutations in this gene, which often leads to severe symptoms including impaired social interaction, repetitive behaviors, and intellectual disability. By using an engineered virus to deliver functional copies of the gene directly into the brains of juvenile mice, scientists observed dramatic behavioral changes within weeks.
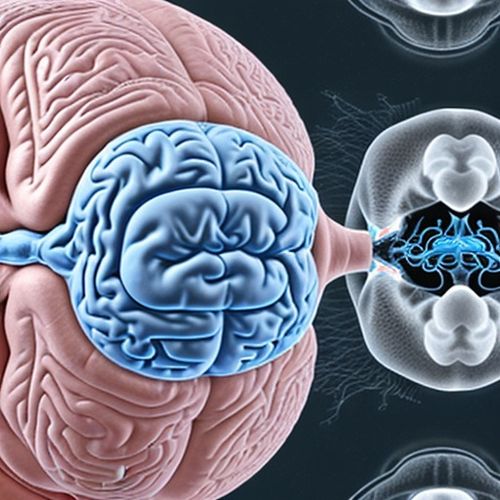
What makes these results particularly remarkable is the age at which intervention proved effective. The therapy was administered to mice that had already developed autism-like behaviors, equivalent to late childhood or adolescence in humans. This challenges previous assumptions that such neurological conditions require intervention during very early brain development. Treated mice showed increased interest in social interactions with other mice, reduced repetitive behaviors, and improved learning capabilities compared to untreated controls.
The research builds upon decades of work identifying genetic contributors to autism. While hundreds of genes have been associated with ASD risk, SHANK3 has remained a prime therapeutic target due to its central role in maintaining the structure of synapses - the communication points between neurons. Mutations in this gene disrupt the brain's ability to process information efficiently, leading to characteristic autism symptoms.
Technical hurdles overcome in this study included engineering a viral vector capable of delivering the relatively large SHANK3 gene and ensuring its expression in the right brain regions at appropriate levels. The team used adeno-associated viruses (AAVs), modified to cross the blood-brain barrier when injected intravenously. This approach avoided the need for invasive brain surgery, potentially making future human applications more feasible.
Behavioral tests conducted eight weeks after treatment revealed striking differences. In social preference tests, treated mice spent about 70% more time investigating unfamiliar mice compared to objects, a ratio similar to healthy controls. They also showed greater variability in their exploration patterns, suggesting reduced rigid thinking. Maze tests demonstrated improved cognitive flexibility, with treated mice adapting more quickly to changed reward locations.
While celebrating these results, the research team emphasized that translation to human therapies will require extensive additional work. The complexity of human autism, which involves multiple genetic and environmental factors, presents challenges that mouse models cannot fully replicate. Furthermore, the treatment only addressed symptoms related to SHANK3 mutations, which account for a small percentage of autism cases.
Ethical considerations also come into play, as gene therapy for neurodevelopmental conditions raises questions about identity and the definition of neurological diversity. Some autism advocates argue that research should focus on accommodations and support rather than biological interventions. However, for individuals with severe impairments affecting quality of life, this breakthrough offers hope for future options.
The next phase of research will focus on optimizing delivery methods, assessing long-term effects, and testing whether the therapy can reverse already-established neural circuit abnormalities. Parallel studies are investigating whether similar approaches might benefit other genetic forms of autism. Clinical trials in humans could begin within 3-5 years if safety studies in larger animals prove successful.
This study arrives at a time of growing recognition that autism comprises many biologically distinct conditions that may require different treatment approaches. The success of gene therapy in this specific genetic form suggests a future where autism treatment may become increasingly personalized based on an individual's genetic profile. As our understanding of autism's biological basis deepens, so too does the potential for targeted interventions that address root causes rather than just symptoms.
Funding for this research came from multiple sources including the National Institutes of Health, several autism science foundations, and biotechnology partners interested in developing genetic medicines for neurological conditions. The interdisciplinary team included neuroscientists, geneticists, virologists and behavioral experts from institutions across North America and Europe.
As with any breakthrough, caution remains essential. The history of autism research includes many promising leads that failed to translate to effective human treatments. However, the specificity of this genetic approach and the robustness of the behavioral improvements in this study have generated cautious optimism in the scientific community. For families affected by SHANK3-related autism disorders, these findings represent a tangible step toward potentially transformative therapies.
The research paper includes extensive supplementary data on molecular and cellular changes observed in the treated mice, showing normalization of synaptic protein levels and improved neural connectivity in brain regions associated with social behavior. These biological correlates provide mechanistic insights supporting the behavioral improvements and suggest the therapy is addressing core pathological processes.
Beyond autism, this work contributes to the growing field of neurodevelopmental disorder therapeutics. The demonstrated ability to modify neural circuits after their initial formation challenges long-held beliefs about the rigidity of brain development. Similar approaches might eventually be applied to conditions like schizophrenia or intellectual disabilities that share some genetic risk factors with autism.
As research progresses, attention will turn to practical considerations: how to identify candidates for such therapies, how to assess risks versus benefits, and how to ensure equitable access if treatments become available. The high costs associated with gene therapy development may present additional barriers that will need addressing through policy and healthcare system adaptations.
For now, the study stands as a proof-of-concept that genetic forms of autism may be treatable through targeted biological interventions. It represents a convergence of advances in gene therapy, neuroscience, and autism genetics that could eventually lead to meaningful improvements in quality of life for certain individuals on the autism spectrum.

By Victoria Gonzalez/Apr 10, 2025
By Joshua Howard/Apr 10, 2025

By Noah Bell/Apr 10, 2025

By Emily Johnson/Apr 10, 2025

By Eric Ward/Apr 10, 2025
By Megan Clark/Apr 10, 2025
By Samuel Cooper/Apr 10, 2025

By Daniel Scott/Apr 10, 2025
By Emma Thompson/Apr 10, 2025

By Rebecca Stewart/Apr 10, 2025
By Lily Simpson/Apr 10, 2025
By John Smith/Apr 10, 2025

By John Smith/Apr 10, 2025
By Samuel Cooper/Apr 10, 2025

By John Smith/Apr 10, 2025
By Rebecca Stewart/Apr 10, 2025
By Joshua Howard/Apr 10, 2025