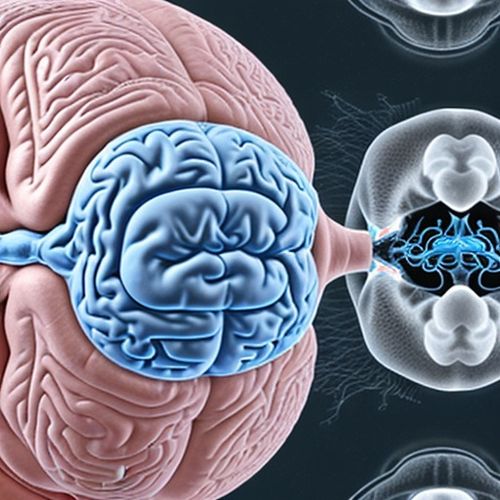
In a groundbreaking development for Parkinson's disease treatment, researchers have successfully demonstrated the potential of focused ultrasound technology to precisely target and destroy malfunctioning brain regions without invasive surgery. This non-invasive approach could revolutionize how we treat neurological disorders, offering hope to millions of patients worldwide who suffer from the debilitating motor symptoms characteristic of Parkinson's.
The technique, called Magnetic Resonance-guided Focused Ultrasound (MRgFUS), combines real-time MRI imaging with highly concentrated ultrasound waves. What makes this treatment remarkable is its ability to penetrate the skull and selectively ablate problematic brain tissue - particularly the overactive globus pallidus or thalamus that cause Parkinson's tremors and dyskinesias - while leaving surrounding healthy tissue intact.
Unlike traditional deep brain stimulation which requires implanting electrodes through risky neurosurgery, this outpatient procedure involves no incisions, no anesthesia, and significantly reduced infection risks. Patients remain fully conscious during the treatment, allowing physicians to monitor symptom improvement in real-time as they precisely adjust the ultrasound parameters.
The science behind this innovation lies in the precise focusing of multiple ultrasound beams. While individual beams pass harmlessly through tissue, their convergence creates enough thermal energy to destroy targeted cells. Advanced MRI thermometry provides continuous temperature monitoring, ensuring safety margins are maintained throughout the procedure.
Clinical trials have shown particularly promising results for patients with medication-resistant tremors. In controlled studies, approximately 75% of participants experienced significant tremor reduction immediately after treatment, with benefits persisting through 12-month follow-ups. Perhaps more importantly, the procedure demonstrated an excellent safety profile, with most adverse effects being mild and transient.
Researchers emphasize that this treatment isn't a cure for Parkinson's disease, but rather a sophisticated symptom management tool. The neurodegenerative process continues, but by interrupting the faulty neural circuits responsible for motor symptoms, patients can regain quality of life and reduce dependence on medications that often cause severe side effects.
Current limitations include the treatment's inability to address non-motor symptoms and the fact that only certain brain targets are accessible with existing technology. The blood-brain barrier presents another challenge, though researchers are investigating whether lower-intensity ultrasound could temporarily open this barrier to deliver neuroprotective drugs.
As the technology evolves, scientists anticipate broader applications for Parkinson's treatment. Future directions include combining lesioning with neuromodulation techniques and developing protocols for bilateral treatments (currently limited to one brain hemisphere at a time). The medical community watches with cautious optimism as this technology matures, potentially offering a middle ground between medication and invasive surgery for appropriate candidates.
The economic implications are noteworthy as well. While the upfront costs of MRgFUS equipment are substantial, the procedure could prove cost-effective long-term by reducing medication needs, hospitalizations, and caregiving requirements associated with advanced Parkinson's. Insurance coverage remains limited but is expected to expand as more clinical data demonstrates the treatment's efficacy and safety.
Patient selection criteria currently focus on those with clearly defined tremor-dominant Parkinson's who have failed optimal medication management. However, as experience grows, clinicians may identify additional subgroups who could benefit. The treatment appears most effective for patients whose symptoms are severe but haven't yet reached the most advanced disease stages.
Looking ahead, researchers are exploring whether this technology could be adapted to target the substantia nigra - the brain region where dopamine-producing neurons degenerate in Parkinson's. While still speculative, such applications could potentially modify disease progression rather than just symptoms, representing a paradigm shift in our therapeutic approach.
For now, focused ultrasound joins the arsenal of tools against Parkinson's debilitating symptoms, offering a ray of hope where options were previously limited. As clinical experience grows and technology improves, this innovative treatment may well become standard care for appropriately selected patients worldwide.

By Victoria Gonzalez/Apr 10, 2025
By Joshua Howard/Apr 10, 2025

By Noah Bell/Apr 10, 2025

By Emily Johnson/Apr 10, 2025

By Eric Ward/Apr 10, 2025
By Megan Clark/Apr 10, 2025
By Samuel Cooper/Apr 10, 2025

By Daniel Scott/Apr 10, 2025
By Emma Thompson/Apr 10, 2025

By Rebecca Stewart/Apr 10, 2025
By Lily Simpson/Apr 10, 2025
By John Smith/Apr 10, 2025

By John Smith/Apr 10, 2025
By Samuel Cooper/Apr 10, 2025

By John Smith/Apr 10, 2025
By Rebecca Stewart/Apr 10, 2025
By Joshua Howard/Apr 10, 2025