In a groundbreaking development for mental health treatment, psychedelic mushrooms containing psilocybin have shown remarkable efficacy in alleviating treatment-resistant depression during Phase III clinical trials. The results, published in The New England Journal of Medicine, suggest that this once-stigmatized compound may soon revolutionize how we approach mood disorders. Researchers across multiple institutions reported that a single dose of synthesized psilocybin, combined with psychotherapy, produced rapid and sustained antidepressant effects in participants who had failed to respond to conventional medications.
The double-blind, randomized study involved over 400 patients across 22 sites in North America and Europe. Unlike traditional antidepressants that require weeks to take effect—if they work at all—psilocybin-assisted therapy demonstrated significant symptom reduction within 24 hours for nearly 60% of participants. Perhaps more astonishing was the durability of these effects: at the 12-week follow-up, 37% maintained remission from depressive symptoms, compared to just 9% in the control group receiving standard SSRIs alongside psychotherapy.
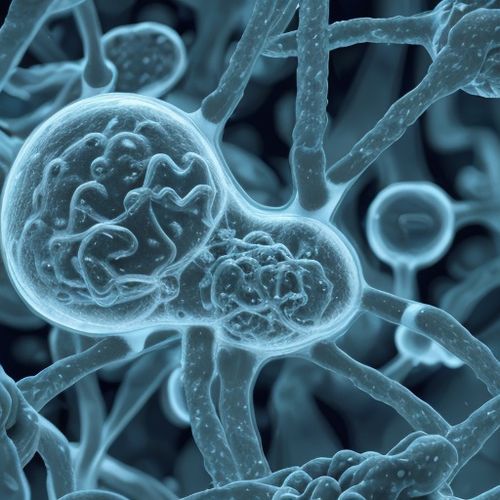
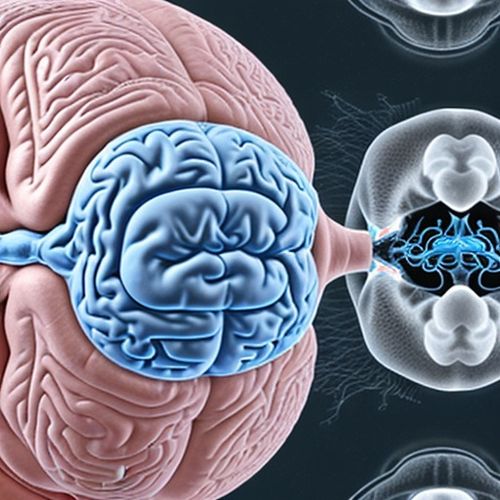
What makes these findings particularly compelling is the mechanism of action. While conventional antidepressants tweak serotonin levels through daily regimens, psilocybin appears to "reset" neural circuits by creating a temporary hyperconnected state in the brain. Functional MRI scans revealed decreased activity in the default mode network—the brain's self-referential "autopilot" system often overactive in depression—while simultaneously increasing connectivity between regions that typically don't communicate. This neurological reorganization, researchers hypothesize, allows patients to break free from rigid negative thought patterns.
The therapy protocol involves careful preparation. Participants undergo multiple psychotherapy sessions before receiving the psilocybin dose in a controlled setting with trained facilitators. The six to eight-hour psychedelic experience is followed by integration therapy to help process insights. "It's not about the drug alone," emphasizes Dr. Rachel Whitaker, lead investigator at Johns Hopkins. "The substance opens a therapeutic window, but the real work happens through the supported psychological journey before and after."
Safety data proved reassuring—no participants experienced serious adverse events, though transient anxiety during the psychedelic session was common. Crucially, unlike ketamine (another psychedelic being explored for depression), psilocybin showed no potential for abuse or dependence in the trial. This safety profile, combined with the lasting effects from just one or two doses, could make it a cost-effective alternative to lifelong pharmaceutical regimens.
Regulatory hurdles remain despite the promising results. The DEA currently classifies psilocybin as Schedule I, alongside heroin and LSD. However, the FDA has granted psilocybin therapy "Breakthrough Therapy" designation twice since 2018, fast-tracking its development. Analysts predict potential approval by 2025 if ongoing trials continue to demonstrate efficacy. Several states including Oregon and Colorado have already decriminalized psilocybin mushrooms, with Oregon launching legal therapeutic use earlier this year.
The implications extend beyond depression. Parallel research shows promise for psilocybin in treating PTSD, addiction, and end-of-life anxiety. As the data accumulates, even traditionally conservative psychiatrists are reconsidering psychedelics. "After decades of stagnant progress in psychiatric medications," notes Dr. Whitaker, "we're witnessing what may become the most significant paradigm shift since the discovery of Prozac." Pharmaceutical companies are taking notice, with Compass Pathways—backed by Peter Thiel—leading commercialization efforts for synthetic psilocybin.
Skeptics caution that more long-term data is needed, particularly regarding how often booster sessions might be required. The therapy's intensive nature (requiring two therapists per patient during sessions) also poses challenges for scaling. Yet for millions battling intractable depression, these trial results offer something scarce in mental health care: hope grounded in rigorous science. As one participant described, "It wasn't just about feeling better—it was about remembering how to be better."
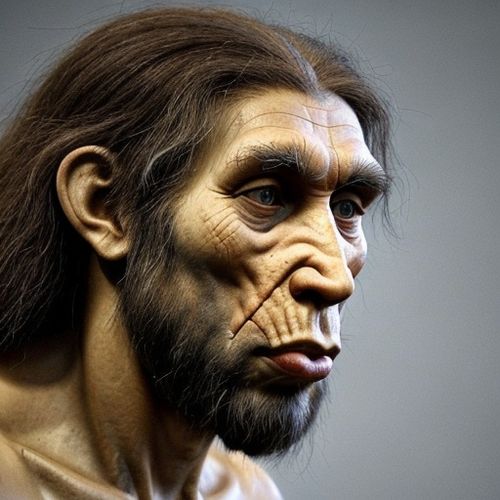
The cultural significance of this research cannot be overstated. Psychedelics, demonized during the War on Drugs, are undergoing rigorous rehabilitation through science. Indigenous communities—who have used psilocybin mushrooms ceremonially for centuries—are finally gaining recognition for their ancestral knowledge. Modern medicine stands at the threshold of integrating ancient wisdom with cutting-edge neuroscience, potentially healing not just individual brains, but our fractured relationship with these powerful compounds.
Looking ahead, researchers aim to identify biomarkers predicting who will respond best to psilocybin therapy. Refinements in dosing protocols and therapist training programs are underway. What began as fringe research two decades ago now commands mainstream attention, with venture capital flowing into psychedelic biotech startups. The mental health crisis demands innovative solutions, and psilocybin—once relegated to counterculture—may soon become a standard tool in psychiatry's arsenal.

By Victoria Gonzalez/Apr 10, 2025
By Joshua Howard/Apr 10, 2025

By Noah Bell/Apr 10, 2025

By Emily Johnson/Apr 10, 2025

By Eric Ward/Apr 10, 2025
By Megan Clark/Apr 10, 2025
By Samuel Cooper/Apr 10, 2025

By Daniel Scott/Apr 10, 2025
By Emma Thompson/Apr 10, 2025

By Rebecca Stewart/Apr 10, 2025
By Lily Simpson/Apr 10, 2025
By John Smith/Apr 10, 2025

By John Smith/Apr 10, 2025
By Samuel Cooper/Apr 10, 2025

By John Smith/Apr 10, 2025
By Rebecca Stewart/Apr 10, 2025
By Joshua Howard/Apr 10, 2025